The prosthetic industry has been around for a long time, but recent innovations in technology are changing the way that prosthetics and orthotics are produced. A prosthetic is a device that “replaces missing body parts or limbs,” while an orthotic “stabilizes, supports, immobilizes, or relieves part of a body or limb, or corrects defective positions.” Both of these consist of functional parts, or joints, and areas that connect with the patient’s body. Due to the level of manual work involved in creating these devices, it is nearly impossible to replicate outcomes. Digital fabrication, however, can eliminate these “unwanted deviations” as it standardizes the process, as well as allows for cost reduction and improved aesthetics.
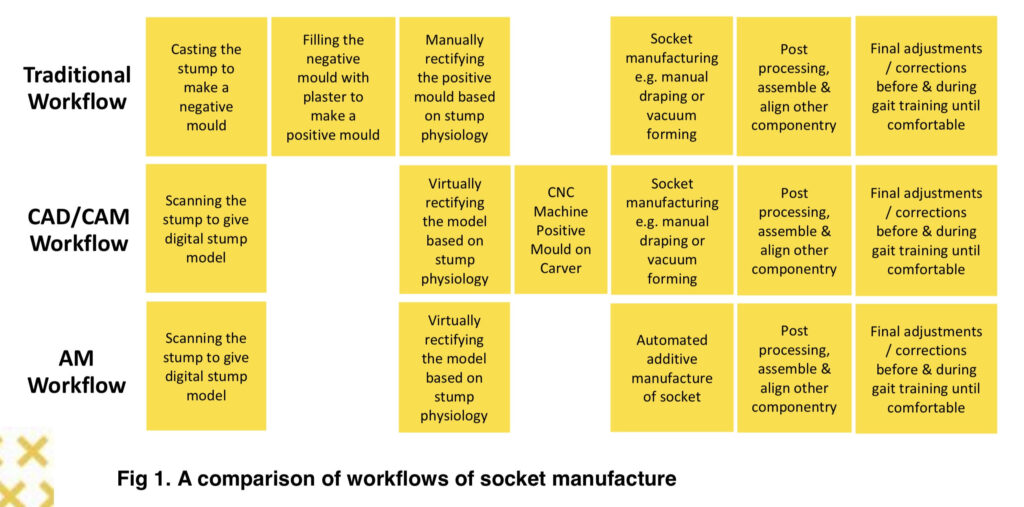
For the traditional workflow, the clinician begins by making a plaster mold of the remaining body part. This is the one area where traditional workflow has an advantage over digital fabrication because the technician can compress soft areas similarly to how the final product would and correct accordingly. Next, they create positive geometry from this cast with plaster. The clinician then adds material where no pressure is needed and takes away where tight connections are needed. This positive form is what is then used as the base for the prosthetic design. This traditional process takes several visits by the patient, so it can become an expensive process due to labor costs for the clinician. There has also been a demand for more complex products with less funding, which has created a search for efficiency. Digital fabrication can reduce the number of steps in this process. The clinician uses a 3D scan to capture the patient’s measurements instead of a cast. They then use this scan to build a digital model to then fabricate with the CNC or 3D printer.
An example of this digital workflow can be seen with prosthetics company Haussler’s development of a prosthetic forefoot shoe. This is a shoe for somebody who has lost all or part of the front of their foot and is a very difficult prosthetic to make because the sole has to be adapted to the weight and gate of each patient. A researcher at Haussler, Anthony Krieger, uses movement analyses and finite element simulation to calculate the perfect sole digitally. He then uses their preferred program, Geomagic Freeform and its Dynabot functionality tool to implement it. Most of this prosthetic is predefined, but size and rigidity are adapted to the patient through the movement analyses and finite element simulation. Previously, this process would have been completed through trial and error along with multiple fitting appointments, resulting in a lengthy and expensive process. With this new technology, however, the process is streamlined, saving time and money.

Dental implants are another example of this digital workflow. It allows clinicians to create solutions for things from single unit abutments, to multi-unit arch supports. For example, there are problems that arise with replicating movements of the jaw through traditional processes now being solved with virtual articulation. The clinician takes a scan of the jaw cast and transfers mechanical articulation into virtual. Software then calculates features needed to adjust the prosthetic to the patient’s jaw movement. This is then fabricated with Cad milling, which removes issues of distortion and porosity created in the lost-wax casting process. Overall, this digital process allows for a major cost reduction.
The last example of digitally fabricated prosthetics is William Root’s Exo-prosthetic leg, which is a “customizable titanium exoskeleton that replicated the exact form of the amputated limb” (Roots). This prosthetic was created due to Root’s belief that the unappealing appearance of prosthetics is a direct result of the outdated production process. The mechanical and robotic look can amplify the sense of loss and psychological state of amputees. The process for creating this prosthetic begins with a scan of the remaining intact limb and the residual limb. The clinician then uses FitSocket technology developed by a biometric lab at MIT to capture the properties of the client’s leg tissue. Next, they use the scan of the remaining limb, residual limb, and standard existing prosthetic mechanisms used to create the 3D model. The model is then hollowed out to reduce weight and form the exoskeleton. This can then be used to create a custom surface pattern, or as a base for a silicone sleeve. The prosthetic is printed out of titanium and the connectors are printed directly onto the skeleton. Through digital fabrication, William Root is able to create a prosthetic more pleasing for the user through the design aesthetics made possible with the digital processes.

A main issue in the prosthetic industry is accessibility. The majority of amputees live in lower to middle income communities (LMIC), but most digital fabrication innovation is happening in high income areas. Five to fifteen percent of people in need of a lower limb prosthetic do not have the access. There is an overall lack of prosthetic service in LMICs that digital fabrication could help with through streamlining and standardizing the process. The question remains though of how feasible is this really? There is a training burden to achieve a full digital workflow because clinicians would then need to take time out of their day of seeing patients to learn these new technologies, so there is a potential of it doing more harm than good. Overall, the industry needs to prove the reliability and quality of materials for additive manufacturing through large scale trials and research to convince these communities to trust the technology.
Overall, digital Fabrication technology results in a more comfortable and customized fit, which is arguably the most important aspect of a prosthetic. If the fit is not correct, it can cause pain, swelling, chafing, and other issues for the patient. It also opens up possibilities for new construction geometries specific to patients’ needs. Additionally, it allows for changes to be more easily made as opposed to with the casting process the professional would need to start over completely to make a change, resulting also in an accelerated idea development. Digital fabrication allows for many improvements to be made in the prosthetics industry, resulting in a better experience for the patient and clinician.